Amanda is a freelance writer. She earned her bachelor’s degree in journalism from the E.W. Scripps School of Journalism at Ohio University.
Treatments target chronic pain and inflammation
On most days for the past 25 years, 79-year-old Arthur Cooper of Park Ridge has experienced side effects stemming from genetic neuropathy, which causes numbness, tingling, and pain throughout the peripheral nervous system.
On good days, like today, Cooper, whose name has been changed for privacy, enjoys doing projects around the house. He had just spent the morning installing a bathroom grab bar for his wife.
Yet, because his pain increases with activity, “I know I’m more than likely going to be in a significant amount of pain tomorrow, especially in my shoulders,” he says. Cooper accepts his pain, but he doesn’t let it rule his life. Last week, he cleaned the garage knowing it could put him out of commission for two to three days.
Chronic pain is among the most common chronic conditions in the U.S. One in five U.S. adults experience chronic pain, according to a recent report in the journal Pain, which looked at data from the National Center for Health Statistics. Lost productivity in the U.S. due to chronic pain costs nearly $300 billion annually, researchers estimate.
In older adults, that pain largely goes undertreated, according to the National Institutes of Health. Older adults don’t always report their pain because they don’t realize it’s treatable or they believe it will lead to more medications and costly tests.
When there’s an injury or infection, the body’s inflammatory response increases blood flow to get more white blood cells to the area. This causes redness, warmth, and swelling that can trigger nerves and cause pain.
“Very importantly, we need to lower the inflammation of the body,” says Jing Liang, MD, a rehabilitation doctor who specializes in pain medicine at Northwestern Medicine Huntley Hospital.
Types of treatment
Older adults are more likely to have chronic pain problems, due to increased rates of cancer and other health conditions. When their pain is poorly managed, they risk suffering, disability, and social isolation.
Treatment for chronic pain aims to improve function and reduce pain during everyday activities. Common approaches include:
Ice or heat therapy. Ice or heat therapy are good options for treating pain directly, says Rahul Khapekar, DO, an attending sports medicine physician at the Joint Relief Institute, which has three Chicagoland locations. “Ice is generally good to decrease inflammation over joints, and heat is good for some chronic pains like tight muscles,” he says.
Physical therapy. Physical therapy, including osteopathic manipulative treatments, can reduce pain by loosening tight joint tissues, improving circulation, and realigning joints and bones. “Rehabilitation with chiropractic treatment or physical therapy and a home exercise program also help patients manage the pain better,” Liang says.
Mind-body modalities. “Mind-body treatments will help patients manage the pain in a more holistic and integrative manner,” Liang says. Approaches include breathing exercises, massage, and acupuncture. Practicing yoga and meditation daily can reduce stress, which in turn lowers inflammation in the body. More specific psychological approaches include biofeedback, hypnosis, and cognitive behavioral therapy.
Pet or music therapies. Some people find relief after engaging in complementary therapies such as animal-assisted therapy and music therapy, which encourage the brain to release calming endorphins.
Medications, supplements, and topical treatments. Some over-the-counter pain medications and products may help with pain relief, including topical gels and ointments, CBD creams, or supplements with turmeric and other spices. Individuals should check with their doctor to make sure the supplements are safe and won’t interact with any of their medications.
Joint injections. Some people try steroid injections, which can decrease inflammation, and hyaluronic acid injections, which help lubricate the joint and reduce friction.
Interventional procedures. Radio- frequency ablation is a minimally invasive procedure that uses heat to reduce transmission of pain signals. It’s used for some neck and low-back pain.
Narcotics and surgery. Narcotic medications can be risky, so they should only be used in select cases for a short period of time, Khapekar says. If conservative, noninvasive methods don’t work, doctors might recommend surgery, depending on the condition. People should discuss with their physician the risks of surgery, as well as the expectations for pain relief.
Considerations
Older adults also should check with their doctor before embarking on a new treatment. Discuss any obstacles to pain management, such as transportation to visits, cost of medications or treatments, and side effects, Khapekar says.
Try one approach at a time, to gauge its benefit before you move on to another option, Khapekar says. It may take several attempts to find the treatment that works best for pain.
For Cooper, using a heating pad on his shoulder helps more than medication. “I’ll leave it on for an hour, and boy, that is so soothing. It’s a big relief knowing you have something to help you. Unfortunately, when it cools off, sometimes the pain comes right back.”
It’s time to seek help from a professional “if you are experiencing pain that is significant enough to interfere with your activity goals, especially with activities of daily living,” Liang says.
Pain, unfortunately, is prevalent in many older adults. But that doesn’t mean people have to accept it. With a variety of treatment options, help may be on the horizon.
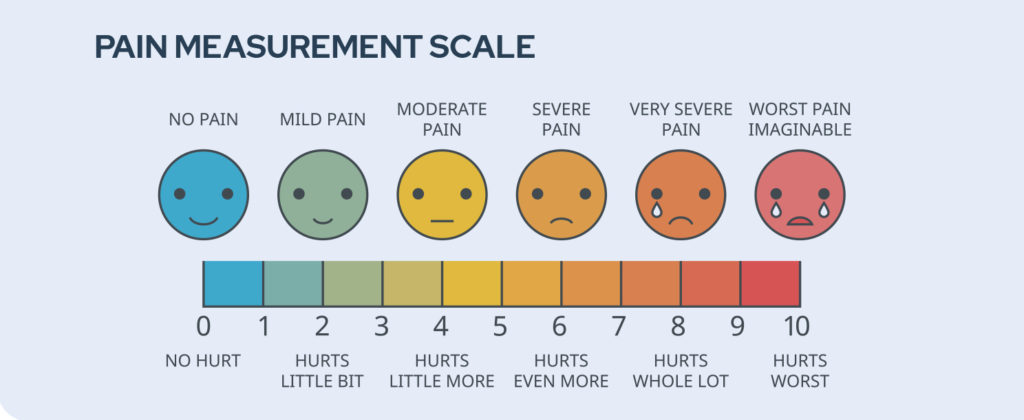
How Bad Does It Hurt?
A common pain scale tool features a series of illustrated faces that gradually progress from smiling (zero: no hurt) to crying (10: hurts worst). A rating of 10 means a person is experiencing the worst pain of their life.
But everyone has a different pain tolerance. So assessing a person’s functional activity can be the best way to determine their pain level, says Jing Liang, MD, a chronic pain specialist at Northwestern Medicine Huntley Hospital.
Rahul Khapekar, DO, an attending physician at the Joint Relief Institute, finds the pain scale useful as a tool to evaluate patients at follow-up visits. There’s not much correlation between your pain and someone else’s, Khapekar says. “But if you rate your pain today and again next week at a follow-up visit, then we’re only comparing your own pain to yourself. That’s where the pain scale shows its value,” he says.