Nancy, who studied and worked in France for 10 years, writes about health, cultural events, food and the healing power of the arts.
The factors that put older adults at risk for falls — and how to prevent them
![]() Fact checked by Catherine Gianaro
Fact checked by Catherine Gianaro
Older adults, especially those who ignore signs of aging, are at risk of experiencing a life-changing fall. Dina Kartsonas, an occupational therapist and partner at FYZICAL Therapy & Balance Centers – Chicago, sees the problem often. She works to rehabilitate older adults who have suffered the consequences of falls because they’re not as steady on their feet as they once were. In fact, 1 in 4 adults over age 65 experiences a fall every year; 1 in 10 of those falls will result in an injury, according to the Centers for Disease Control and Prevention.
Magadena Bednarczyk, MD, division chief for geriatrics and palliative medicine at Rush University Medical Center, says older adults’ falls have increased in the past five years. “I think that as a consequence of the Covid pandemic, the habits and lifestyles of older adults were disrupted, which resulted in increasing their isolation and limiting their mobility,” she says. “That lack of activity and also the loss of their muscle mass due to aging resulted in more falls.”
Some injuries, such as hip fractures, can have a long-term physical impact. “Even when older adults recover from hip fractures, they may never recover to their pre-fracture level of independence and may need caregiving at home or an alternative living arrangement with more assistance available to them, like assisted living,” Bednarczyk says.
Those experiences can have a long-term psychological impact as well. “When older adults fall, they lose their confidence and are afraid they are going to fall again so they limit their mobility, remain home-bound, and therefore increase their risk of falling,” Bednarczyk says. “Physical therapy can help them regain their strength but also rebuild their confidence.”
They just have to commit to the physical therapy exercises on their own after they are no longer working with a physical therapist to maintain the benefits, Bednarczyk says.
Who’s at risk?
Though fall risks increase with age, falls are not inevitable. Kartsonas, a member of the Fall Prevention Coalition with the University of Illinois, offers fall prevention workshops. “Older adults should be aware of the risks they face, so they can prevent the danger of falling,” she says.
A fall could be caused by one of their medications, or by the interaction of certain medications taken together — a risk especially if different specialists are prescribing medications for the person. Kartsonas says that older adults should ask their pharmacist to review all of their medications and note any that cause dizziness or a drop in blood pressure.
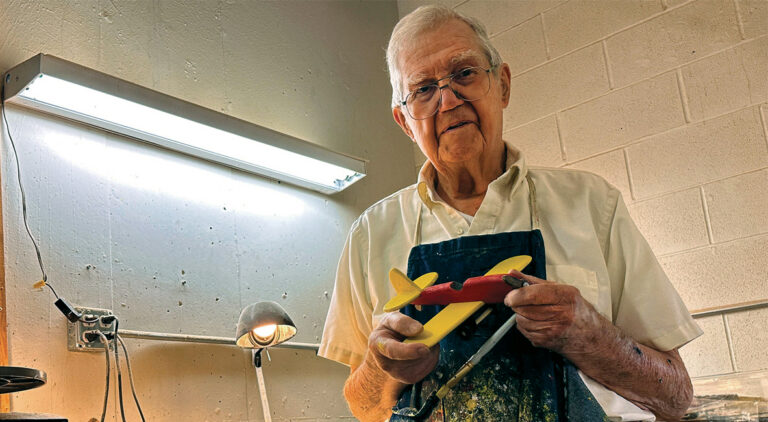
Certain medical conditions can also involve the risk of falling. About two and a half years ago, Bob Blaida, 69, started feeling like he was losing his sense of balance and was especially fearful of falling when he turned his head very quickly. He stopped riding his bike regularly because he felt it was too dangerous. He knew he had to give up water skiing, too.
Blaida consulted a doctor who diagnosed him with early stage Parkinson’s disease. The doctor told him about the negative implications of the disorder’s unintended movements and impacts on coordination and balance. He retired from his work in sales and sought out a second doctor who specialized in mobility.
“He told me the best thing I could do to slow the progression of the disease and maintain my quality of life was to exercise,” Blaida says. One good option: boxing.
Blaida signed up at Rock Steady Boxing in Naperville where he could relate to the participants who were in the early stages of Parkinson’s. He now goes there three times a week. The one-hour class focuses on hand-eye coordination, strength training, flexibility, and speed. “It’s a full body workout,” he says.
In addition, Blaida started working with Kartsonas at FYZIcal because she specializes in balance issues and also has a certification in Parkinson’s disease. During the five months they worked together, Blaida learned that one of the reasons he felt like he was going to fall was because the left side of his body had become weaker than the right side. He focused on building strength there to improve his balance.
In addition to his boxing class, Blaida walks three times a week in his Naperville subdivision. “I realized that the fire hydrants are equal distance apart, so I keep adding more and more hydrants to increase the distance I walk,” Blaida says. “I love TV and could sit on the couch all day watching it, but I can’t afford to do that.”
Fall prevention measures
For older people who want to take a class or follow an exercise regime to prevent falls, Kartsonas suggests to first consult with a physical therapist to evaluate their strengths and weaknesses and help develop a plan to address specific fall risks.
Tai chi and yoga are worth exploring as well. “Research shows that [tai chi] can prevent falls by up to 50%,” Bednarczyk says. “It uses slow-paced, gentle, full-body movements to promote good balance and strengthens the muscles and the bones. It improves your core and gives you a good range of motion to do daily tasks.”
The senses are also essential to balance because they let us know where we are in the world. Older adults should have their vision and hearing checked regularly.
On the topic of screenings, Bednarczyk says that screening for osteoporosis, the loss of bone density, is a must. The disease has no obvious symptoms, but it results in fragile bones that can break easily during a fall. If osteoporosis is detected, medical treatment is available.
Dehydration is another common risk that can be avoided. “As we grow older, we lose our sense of thirst, so by the time older adults feel thirsty, they can already be dehydrated, which causes fatigue and a risk of falling,” Bednarczyk says.
Older adults also struggle with bladder control, so they may drink less to urinate less. But that could also lead to dehydration. “As a strategy, they can just drink more in the morning or early afternoon when they are home,” Bednarczyk says.
Supportive footwear can prevent falls, too. Some women in their 80s and 90s come to appointments with Bednarczyk wearing 3-inch high heels. “They take pride in being well dressed,” she says. “They don’t want to give up those shoes, so it takes a lot of negotiating to get them to change to 1-inch heels.”
For older adults, cutting their toenails can become difficult or impossible, and they end up risking falls because it becomes painful to wear shoes. Others wear shoes that have become too loose, or slippers without support or rubber soles for traction.
Karsonas recommends well-fitting, slip-on shoes. In general, she says, “The soles should allow the person to feel the surface they are walking on so they can adapt to different textures such as soft carpeting, cement sidewalks, and grass.”
Although it may be trite, Bednarczyk says there is one phrase that underscores the importance of preventing falls. “It’s survival of the fittest,” she says.