Lisa Fields covers health, psychology, nutrition, fitness, and eldercare for Reader’s Digest, AARP, Next Avenue, and other publications.
Managing the risks of multiple medications
More is not always better — especially when it comes to medications. Taking too many medications increases the risk for adverse drug reactions — a particularly acute problem for older adults.
Adults age 65 and older visit the emergency department three times more often for medication-related adverse events than younger adults do, according to the Centers for Disease Control and Prevention.
The chance of problems increases when someone takes more than five medications, but many older adults easily surpass five medications daily. That’s because they’re more likely to have chronic diseases — diabetes, heart disease, and cancer, to name a few — that require multiple medications.
Research published in the journal American Family Physician shows that some doctors may prescribe medications extraneously. Sometimes, they continue prescribing medication that a person no longer needs. Other times, they prescribe medication solely to counteract side effects of another drug, which increases the number of medications the person is taking and potentially creates more side effects.
“It’s this terrible snowball effect: You start on one medication for a problem. It causes a side effect, so then you’re on a second medication because of that side effect. And then that medication causes a side effect, so you add a third medication,” says Erika Hutz, DO, a geriatrician with Swedish Medical Group in Chicago.
Working with a doctor to eliminate unnecessary medications may help your loved one avoid complications.
“Confusion, falls, and dizziness are our biggest concerns with many medications, especially with individuals who have heart disease, lung problems, breathing problems, or cognitive impairments,” says Ashley Okray, a physician assistant in geriatric services for Rush University Medical Group in Chicago.
Medication complications
Reactions to multiple medications may happen for numerous reasons, including:
· Physical changes. Older adults don’t metabolize medicine the way that they did decades ago. “As you get older, your kidneys shrink in size, and your liver can shrink in size,” Okray says. “The way you break down these medications as an older adult compared to when you were a younger adult can change, predisposing you to side effects and interactions.”
· Human error. It can be difficult to remember to take medication as directed, especially when someone breaks from routine, such as when they travel or are sick. Skipping doses or accidentally double dosing may cause problems.
· Being on autopilot. Prescribing information may change, or individuals may no longer need certain medications, but their doctors don’t always tell them to stop. For instance, doctors no longer recommend baby aspirin, an over-the-counter blood thinner, for most people without cardiovascular disease, due to the risk of bleeding.
“If they fall and if they are bleeding, there is more chance they will end up in better shape [without] the aspirin,” says Manharkumar Patel, MD, a family medicine specialist with OSF Medical Group in Palos Heights.
· Withholding information from physicians. People may not tell doctors that they’re taking dietary supplements or over-the-counter medications, some of which interact with prescription drugs. “A lot of patients say, ‘Oh, this is over-the-counter, so it can’t be bad for me,’” Hutz says. “But there are so many over-the-counter medications that older adults should not be on. For example, pretty much all of the sleep aids are a really bad idea.”
· Counteracting another drug’s side effects. Watch out for unintended consequences. For instance, prescription- strength ibuprofen may cause gastrointestinal problems, so a doctor may prescribe a proton pump inhibitor (PPI) to reduce stomach acid levels. But long-term use of PPIs may cause osteoporosis — which potentially could require additional medication.
Minimize Multi-Drug Complications
Taking too many drugs increases the possibility of adverse reactions and mix-ups. Try these tips to help with medication management:
+ Use a compartmentalized pill box. Choose a pill case with slots for morning, afternoon, evening, and bedtime for every day of the week. Your loved one will be less likely to skip doses, mix up pills, or take medicine twice if it’s clear which pills to take. Fill the pill box for them if they experience confusion. For good measure, set medication reminders on your phone, and check to make sure that the appropriate slots are empty.
+ Get a medication review. Whenever you take your loved one to the primary care physician, bring along every medication that they take, including over-the-counter drugs and supplements. The doctor can see what is necessary and what may be eliminated.
Once a year, ask whether all of the medication is still necessary. If the drug is necessary but you’d like fewer pills, see if your loved one is eligible for extended-
release medications, which are taken once a day
instead of more often.
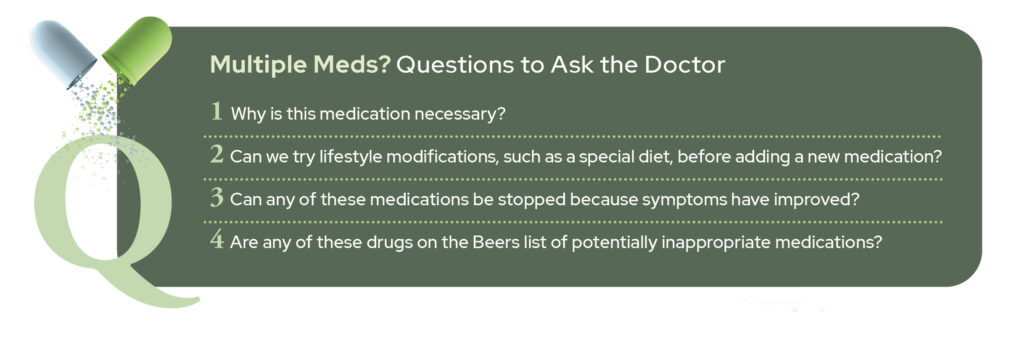
+ Consult the Beers list. The American Geriatrics Society’s Beers Criteria for Potentially Inappropriate Medication Use in Older Adults lists medications that may not be safe. Check online to see if any of your loved one’s drugs are on the list, or ask the doctor.
“Ideally, older adults would not be on any of these medications, but sometimes it’s necessary,” says geriatrician Erika Hutz, DO. “I would bring [a medication] to my physician and say, ‘I heard about the Beers list, and I see that Mom is on this medication. Is this something that she really needs to be on? Or is there an alternative?’”