Ezra is a journalist and editor based in Chicago. He specializes in long form, enterprise reporting, solutions stories and environmental topics. From the high peaks of the west to the Blue Ridge in the south, Ezra loves the outdoors and takes every opportunity to trade the flatness of Illinois for a trip to the mountains.
How care teams help patients come to terms with adverse health news
Two and a half years ago, Yvette Lamphier was not feeling well. Of all the possibilities going through her mind of what it could be, cancer was the last.
When she received the call from her doctor at work, she broke down in tears. A single mom, Lamphier thought of her 18-year-old daughter. What was she supposed to do?
“Your life just kind of stops,” she says. “It was fear, disbelief, so many emotions all at one time. Then, the next moment, you’re thinking you have to tell your daughter and your family.”
Lamphier was treated at City of Hope Chicago by Barbara Buttin, MD. A gynecologic oncologist, Buttin primarily treats patients who have little hope of recovery. Though many patients have positive outcomes, not every case has a magic-bullet cure, and that’s when Buttin must have the difficult conversation to end treatment.
“That’s just part of the job,” Buttin says. “You have to know, when you reach that point, when it makes sense to push, and when it may even be harmful to the person to do more. It’s a very fine line.”
Julie Fitzgerald, MD, a pediatric critical care physician, and Rev. Michael Hayes, a chaplain, work together at Loyola Medicine. Fitzgerald says that combining medical treatment with compassionate care makes for the best support. In pediatrics, people come to her scared and angry. Having a chaplain such as Hayes to turn to helps patients receive more support.
Chaplains can serve in a way as a translator or intermediary to the care team. “They can be the one to transition and take over when we have to step away,” Fitzgerald says. “You simply cannot do the job without that kind of partnership.”
Preparing for difficult conversations with patients and family members works best when the doctor and chaplain prepare together. But Hayes and Fitzgerald don’t work from a script, which keeps their conversations with people genuine.
“I don’t try to come in with any preconceived notions,” Hayes says. “Sometimes you’re just wisest not to do anything that’s canned. Just be there so you can respond to their actual needs.”
Hayes recalls an instance when a boy and his mother had been in a car crash. He watched as the attending doctor rushed in to speak with the boy’s family. The boy wasn’t going to survive, the doctor told them. The family was devastated and the mother severely shocked.
Next, Fitzgerald stepped in. Hayes and Fitzgerald worked together to find the best way for the mother to say goodbye to her son as he passed.
“If you get it right, you earn the trust of the family,” Hayes says. “If you get it wrong, it’s hard to do anything to regain it.”
When options run out and treatment is no longer feasible, Fitzgerald offers a few simple things to provide the best support possible.
“Honesty is really important,” she says. “What I can offer and what I will promise is peace and comfort and dignity. We may not be able to cure, but we can always care.”
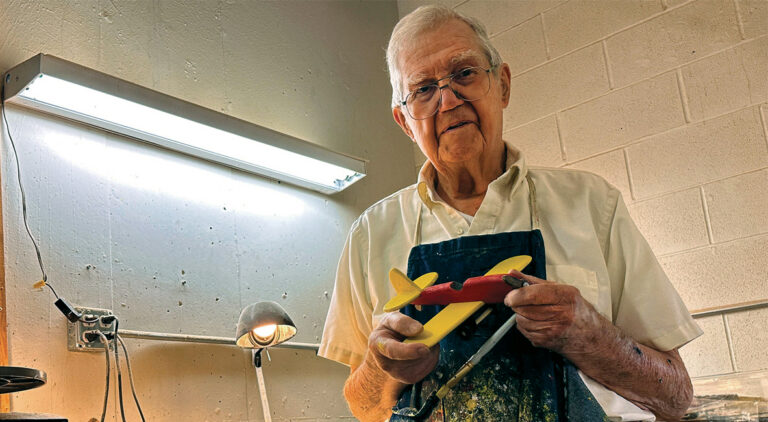
Lamphier was given six to eight months to live. Having a compassionate care team in Buttin and the support of her daughter has helped her persevere through the difficult treatment process. Additionally, being around other patients in similar positions helped Lamphier feel less alone. She made friends, establishing a community to help each other through.
“You find the small wins,” Lamphier says. “But I’m also allowing myself to grieve. I felt I had to stay strong, I couldn’t let anyone see that side of me, but I learned that would affect me negatively.”
Buttin says she sets goals with her patients to make sure their quality of life is the best it can be. When necessary, she prepares her patients with the possibility that there may not be a positive outcome. She also includes the patient’s family or friends in this process, so everyone is on the same page, and the patient has the most support possible. In each situation, Buttin wants everyone involved to be aware of the negatives, to avoid surprises, and be as prepared as they can be for whatever happens.
When it comes to terminal patients, Buttin says stopping treatment early, when there are no more options, is the best way to ensure the last bit of their lives can be enjoyed.
“All the preparative care services, such as hospice services, can enhance your quality of life. They reduce the stress on the body, which will help you feel better and then ultimately will help you transition without stress and fear and pain,” Buttin says.
Sometimes, she adds, patients are surprised by how much more life they gain, at the end of life.